What Causes Varicose Veins?
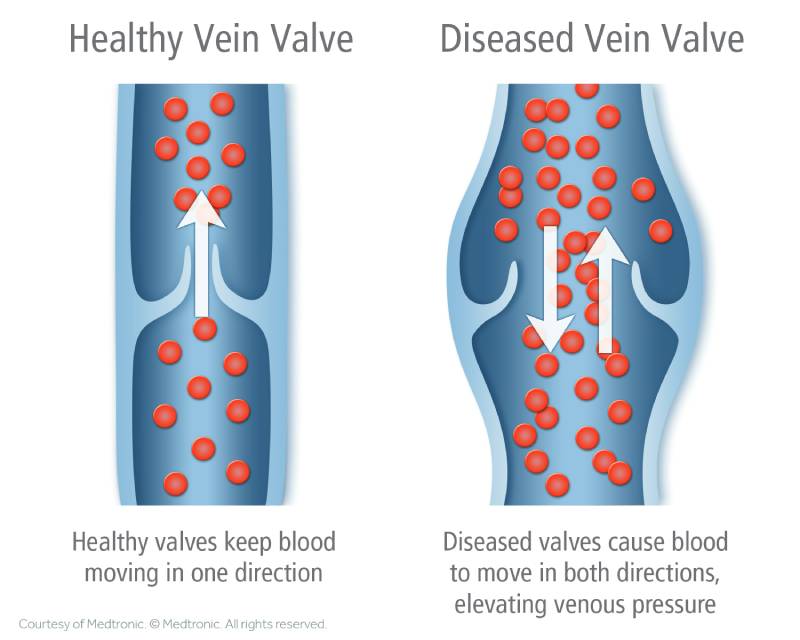
Varicose veins in the legs form when valves in the veins stop working properly. Without a fully functioning valve, the blood struggles against gravity to travel up the leg veins back up to your heart. Blood pools, stretching the vein and leading to bulging, twisting, and discomfort. You may be able to see these veins on the surface, but sometimes the affected veins are slightly below the surface and can only be seen with an ultrasound scan.
But what leads to the weakening of these valves? Why does the blood circulation struggle against gravity and lead to these bulging, unsightly, uncomfortable veins?
Why You’re at Risk for Developing Venous Disease
Age is a common factor with most health conditions, and venous disease is no exception. As we age, certain bodily functions weaken; this includes the vein walls and valves. If you have limited mobility or other medical conditions, this can also increase your risk. Typically, we consider you at a higher risk for developing varicose veins if you’re over 65 years old but it is not uncommon to begin seeing veins or having symptoms of vein disease much earlier. The earlier their onset the worse they tend to get over time.
Pregnancy can also lead to venous disease in a number of ways. The extra weight puts pressure on your veins and can cause them to become varicose. However, you may be surprised to learn that the risk starts even earlier due to hormonal shifts to sustain a healthy pregnancy. These hormones slow your circulation, which can cause the blood to pool in the veins, leading to varicose veins and even blood clots. Plus during pregnancy, as a Mom, your blood volume increases to provide for your growing baby.
Being overweight or obese is also a common cause of venous disease. The extra weight puts pressure on the veins and valves, making them work harder to circulate blood back up to the heart. This extra strain can cause them to become varicose.
Standing or sitting for long periods of time is what causes varicose veins in many individuals. Between modern-day sedentary lifestyles and jobs that require sitting or standing for long periods of time, many patients fall into this category. When you’re immobile for a long time, your calf muscles aren’t doing the work to aid in healthy circulation. The calf muscles are the primary ‘pump’ that returns the venous blood back to your heart. When the pump is idle your veins and valves have to work harder to compensate for the lack of movement, wearing them out faster and leading to venous disease
Varicose veins are also hereditary. If you have a family history of varicose veins (think about your parents and grandparents), you are more likely to develop them yourself. But even if you don’t have a family history you may still have vein problems. So if you have symptoms of vein disease you should get checked out even if you don’t ‘see’ any bulging veins or spider veins on your legs.
Prolonged bed rest is a major culprit in venous disease. It’s where a lot of very fit and active individuals will often get tripped up and find themselves with varicose veins or blood clots. If you are injured, have surgery, or are on prolonged bed rest for any reason, leaving you less mobile, you can develop venous disease. Thankfully, surgery centers have gotten better about making sure if you are at risk that preventive measures are taken. These can include wearing compression stockings while you are in the hospital following surgery or during prolonged hospital stays to help combat this problem. Other options include intermittent compression pumps during your procedure, early ambulation, and in certain cases blood thinners.
Certain health conditions and medications, including over-the-counter and prescription, can increase your risk of developing venous disease. Most chronic illnesses or disabilities that lead to a more sedentary lifestyle or bedrest will increase your risk of developing varicose veins. Prescription hormones, like birth control and testosterone replacement therapy, are common culprits that can increase the risks of blood clots. It’s important to discuss how your health history can increase your risk of venous disease and other health concerns with your physician.
Women are more likely to develop venous disease than men. This is likely due to hormonal shifts, multiple pregnancies, and birth control. Word to the wise, ladies, high heels also play a role in venous disease progression.